|
|
| (One intermediate revision by the same user not shown) |
| Line 1: |
Line 1: |
| | == Clinical Summary == | | == Clinical Summary == |
| | + | This 77-year-old white male with a past medical history of severe osteo- and rheumatoid arthritis went to his internist for increasing joint pain and was started on a new medication containing a narcotic analgesic, acetaminophen, and a non-steroidal anti-inflammatory agent. The patient also self medicated with acetaminophen. Two days later he went back to his doctor complaining of nausea and vomiting, right upper quadrant pain, anorexia, and confusion. Lab evaluation revealed massively increased liver enzymes. The patient went into DIC and died in fulminant liver failure. |
| | | | |
| − | This 77-year-old white male with a past medical history of osteo- and rheumatoid arthritis went to his internist for treatment of increasing joint pain and was started on a muscle relaxant, a narcotic analgesic that also contained 650 mg of acetaminophen, and a non-steroidal anti-inflammatory agent. The patient's medical record also indicated that he self medicated with acetaminophen. Two days later he went back to his doctor complaining of nausea and vomiting, right upper quadrant pain, anorexia, and confusion. Lab evaluation revealed increased liver function tests (AST, 2190; ALT, 1959; LDH, 5020; alkaline phosphatase, 120; GGT, 125; total bilirubin, 3.9). Hepatitis serologies were negative. The patient's blood acetaminophen level was 45 mcg/dL. Over the next several days the patient began to develop petechiae which progressed to ecchymosis and necrosis of his hands and feet. Laboratory studies revealed that the liver function was improving, but coagulation studies were consistent with DIC (platelets, 19,000; FDP, greater than 40; fibrinogen, 90; PTT, 26). The patient was treated with heparin, cryoprecipitate, fresh frozen plasma, and anti-thrombin III. Despite improvement in his coagulation parameters, the patient appeared to have ongoing thrombosis. The patient was evaluated by orthopedic and vascular surgery who recommended bilateral below-the-knee amputations and bilateral hand amputations. However, the patient was found apneic and, in keeping with his request that he not be resuscitated, no resuscitative measures were undertaken.
| + | At autopsy the liver had large areas of pale softened tissue indicative of liver necrosis. |
| − | | |
| − | == Autopsy Findings ==
| |
| − | There were petechia and ecchymoses all over the body. The skin on the hands, feet, and in patches over the entire body was deep purple, the epidermis was friable and there were large areas of desquamation. The fingertips and toes were black and dry. The liver had large areas of pale softened tissue indicative of liver necrosis.
| |
| | | | |
| | == Images == | | == Images == |
Clinical Summary
This 77-year-old white male with a past medical history of severe osteo- and rheumatoid arthritis went to his internist for increasing joint pain and was started on a new medication containing a narcotic analgesic, acetaminophen, and a non-steroidal anti-inflammatory agent. The patient also self medicated with acetaminophen. Two days later he went back to his doctor complaining of nausea and vomiting, right upper quadrant pain, anorexia, and confusion. Lab evaluation revealed massively increased liver enzymes. The patient went into DIC and died in fulminant liver failure.
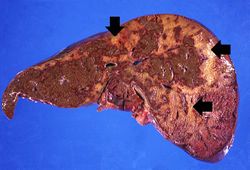
At autopsy the liver had large areas of pale softened tissue indicative of liver necrosis.
Images
This gross photograph of the liver from this patient demonstrates the pale areas of necrosis (arrows).
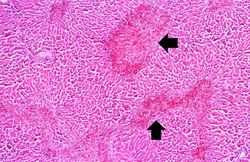
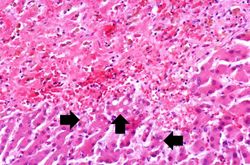
In this photomicrograph of the liver from this patient there are areas of hemorrhagic necrosis (arrows).
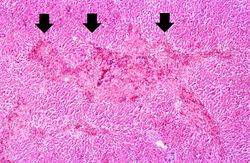
This is another example of the areas of hemorrhagic necrosis (arrows).
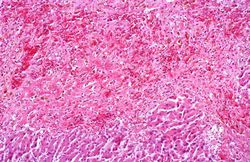
This is a medium-power photomicrograph of the areas of hemorrhagic necrosis. Note the coagulation necrosis and hemorrhage in this area. Viable hepatocytes can be seen along the edge of this lesion.
This is a high-power photomicrograph of the edge of the necrosis. Again, note the coagulation necrosis and hemorrhage in this area. The viable hepatocytes at the edge of this necrosis are vacuolated (arrows).
Photograph taken at autopsy demonstrating the severe necrosis of the skin of foot.
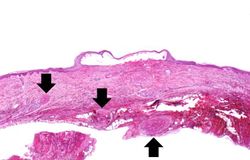
This low-power photomicrograph of the skin from this patient shows a blister and numerous thrombosed vessels (arrows) in the dermis.
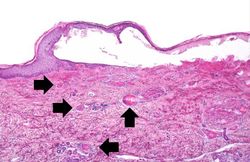
This is a higher-power photomicrograph of the skin from this patient showing a blister and the thrombosed small vessels (arrows) in the dermis.
Virtual Microscopy
Liver: Acetominophen Toxicity
Normal Liver
Study Questions
The acetaminophen level on admission was not elevated; however, the patient had been in distress for some time and had not taken any acetaminophen within the previous 12 hours. Upon questioning, the patient admitted that he had continued to take his usual doses of acetaminophen even after his internist put him on new drugs. He was unaware that one of the new drugs he was taking had acetaminophen in it. Thus, he was taking an overdose of acetaminophen and this resulted in hepatic toxicity.
Adverse drug reactions can occur with therapeutic agents, but in this case the most probable cause for liver necrosis was the unintentional overdose of acetaminophen by this patient who was not aware that one of the new drugs he was taking already contained acetaminophen.
Liver necrosis releases thromboplastin and can initiate the coagulation cascade leading to intravascular coagulation.
Additional Resources
Reference
Journal Articles
Images
Related IPLab Cases