Clinical Summary[edit]
Approximately four months prior to admission, this 68-year-old male began having "sharp, shooting pains" in the lower abdomen. A barium enema at that time was reported as normal. Two months later, the barium study was repeated because of persistent diarrhea and showed a filling defect in the transverse colon. The patient refused to undergo an exploratory laparotomy. During the week prior to this admission, the patient had recurrent diarrhea, cramping abdominal pain, and marked rectal bleeding. He was hospitalized and required 2500 ml of blood to return his hematocrit to normal. A colectomy was done from the hepatic flexure to the rectosigmoid.
Autopsy Findings[edit]
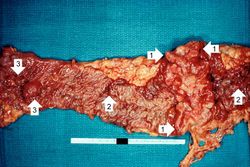
The segment of colon contained numerous polyps and an annular tumor which was 6.7 cm in diameter. Proctoscopic examination of the ascending colon revealed two more polyps which were removed.
This is a gross photograph of the adenoma from the surgical specimen in this case. Note the large, ulcerated, fungating annular (encircling) carcinoma (1) with areas of hemorrhage (2). Also note the adenomatous polyps (3).
This is a closer view of the previous image demonstrating the raised, annular carcinoma (arrows).
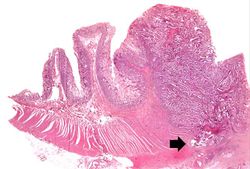
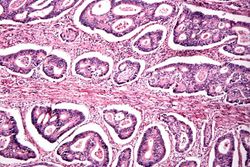
This photomicrograph of the surgical specimen shows the transition between normal mucosa on the left and carcinoma which is invading the wall of the bowel (arrow).
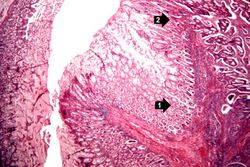
This is a higher-power photomicrograph of the area of transition between the normal (1) and the neoplastic (2) epithelium.
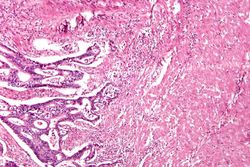
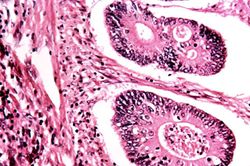
This is a high-power photomicrograph of tumor cells invading the underlying muscularis.
This is a high-power photomicrograph of tumor cells forming glands.
This is a high-power photomicrograph of tumor cells forming glands.
This gross photograph from another case demonstrates an ulcerated adenocarcinoma (arrows) at the rectosigmoid junction.
This is a segment of distal colon from another case. Note the annular tumor that severely compromises the lumen of the colon. There is dilation of the colon proximal to the tumor.
Study Questions[edit]
The peak incidence for colorectal carcinoma is age 60 to 70 years; fewer than 20% of cases occur under 50 years of age. When colorectal carcinoma is found in a young person, pre-existing ulcerative colitis or one of the polyposis syndromes must be suspected.
The clinical presentation depends upon the site of the tumor. Colorectal cancers remain asymptomatic for years. Cecal and right colonic cancers most often lead to fatigue, weakness, and iron-deficiency anemia. These fungating lesions bleed easily and may be discovered at an early stage, provided that the colon is examined thoroughly radiographically and during colonoscopy. Left-sided lesions produce occult bleeding, changes in bowel habit, or crampy left lower quadrant discomfort. In theory, the chance for early discovery and successful removal should be greater with lesions on the left side because these patients usually have prominent disturbances in bowel function, such as melena, diarrhea, and constipation.
Almost all colorectal carcinomas begin as in situ lesions within adenomatous polyps; however, they evolve into different morphologic patterns. Tumors in the proximal colon tend to grow as polypoid, fungating masses that extend along one wall of the capacious cecum and ascending colon. Obstruction is uncommon. When carcinomas in the distal colon are discovered, they tend to be annular, encircling lesions that produce so-called napkin-ring constrictions of the bowel. The margins of the napkin ring are classically heaped up, beaded, and firm, and the midregion is ulcerated. The lumen is markedly narrowed, and the proximal bowel may be distended.
Dietary factors that may predispose to cancer are
- a low fiber diet,
- high intake of refined carbohydrates,
- high fat diet, and
- decreased intake of protective vitamins.
It is thought that reduced fiber content leads to decreased stool bulk, increased fecal transit time in the bowel, and an altered bacterial flora of the intestine. Potentially toxic oxidative byproducts of carbohydrate degradation by bacteria are therefore present in higher concentrations in the small stools and are held in contact with the colonic mucosa for longer periods of time. More recent epidemiologic data have raised some doubt about the importance of fiber in the diet but most nutritionalists still recommend high fiber diet to help prevent colon cancer. Moreover, high fat intake enhances the synthesis of cholesterol and bile acids by the liver, which in turn may be converted into potential carcinogens by intestinal bacteria. Refined diets also contain less vitamins A, C, and E, which may act as oxygen radical scavengers.
Additional Resources[edit]
Reference[edit]
Journal Articles[edit]
Related IPLab Cases[edit]